Abstract
Background: Chromosome 14q32 rearrangements involving the immunoglobulin heavy chain gene (IGH) affect less than 5% of chronic lymphocytic leukemia (CLL) patients. Their clinical course is aggressive and the outcome, worse than other CLL subtypes (Cavazzini et al, 2008; Gerrie et al, 2012). However, the biology of CLL showing IGH rearrangements (CLL-IGHR) is not completely defined. The identification of novel recurrent mutations in CLL by next generation-sequencing (NGS) has offered a more comprehensive view into the genomic landscape of the disease and improved the prognostication of CLL. Thus, mutational analysis might be especially useful in those patients with uncertain prognosis, such as those carrying IGH rearrangements.
Aim: To analyze the mutational profile of CLL-IGHR patients by targeted NGS in order to improve our understanding of the genetic underpinnings of this subgroup.
Methods: The study was based on 899 CLL patients, well characterized at cytogenetic, biological and clinical level, forty-two of them (4.7%) showing IGH rearrangements. Targeted NGS was performed in 231 CLL samples: 117 with 13q deletion, 27 with 11q deletion, 26 trisomy 12, 42 showing IGH rearrangements and the remaining 19 without any cytogenetic alteration. CD19+ B cells were isolated and DNA extracted. SureSelectQXT targeted enrichment technology and a custom-designed panel (MiSeq, Illumina), including 54 CLL-related and recurrent mutated genes, was carried out. The panel yielded 100x or greater coverage on 97% of the genomic regions of interest and the mean coverage obtained was 600x. Mutations were detected down to 3% allele frequency.
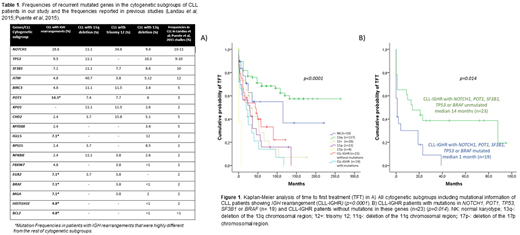
Results: The mutational analysis of CLL-IGHR patients identified a total of 72 mutations in 32 genes. Seventy-one percent of patients (30/42) harbored at least one mutation. The most frequently mutated genes in this cohort were NOTCH1 (28.6%), POT1 (14.3%), TP53 (9.5%), SF3B1 (7%), BRAF (7%), EGR2 (7%), IGLL5 (7%) and MGA (7%), followed by BCL2, HIST1H1E and FBXW7 (4.8%), uncommonly mutated genes in CLL at these frequencies (Table 1). In fact, mutations in NOTCH1, BRAF, EGR2, BCL2, HIST1H1E and FBXW7 were significantly associated with CLL-IGHR patients (p=0.013, p=0.003, p=0.021, p=0.038, p=0.038 and p=0.021 respectively).
In terms of time to the first therapy (TFT), CLL-IGHR had an intermediate-negative impact (median TFT=24 months) compared to the presence of cytogenetic alterations associated with good prognosis such as 13q deletions (median TFT>120 months; p<0.0001) (Figure 1A). Furthermore, the presence of mutations in the most frequently mutated genes (NOTCH1, POT1, TP53, SF3B1 or BRAF) within patients with IGH rearrangements had a negative clinical impact in the TFT and allowed us to refine the prognosis of this subgroup. Thus, the median TFT of patients with mutations was 1 month while the median TFT of patients without mutations was 14 months (p=0.014) (Figure 1B).
A total of 17 out of 42 CLL-IGHR patients (40.5%) carried the t(14;18). Interestingly, patients with t(14;18) were characterized by: 1) A lower mutation frequency (average of mutations/patient=1.05) than the rest of rearrangements with unknown partners (average=2.16; p=0.039), and 2) The presence of mutations in BCL2 (11%) and HIST1H1E (11%). By contrast, CLL-IGHR without BCL2 rearrangement showed mutations in POT1 (20%), TP53 (16%), SF3B1 (12%) and BRAF (12%). Moreover, t(14;18) was significantly associated with good prognosis markers such as the mutated status of the variable region of the immunoglobulin genes (IGHV-M) (p=0.002). However, there was no significant difference in terms of TFT between patients with t(14;18) and patients with other IGH rearrangements (p=0.27).
Conclusions: CLL patients with IGH rearrangements showed: i. A high gene mutation frequency; ii. A distinct mutational profile, with recurrent mutations in POT1, EGR2, BRAF, IGLL5 and MGA genes; iii. An adverse clinical outcome refined by the negative effect of genetic mutations. iv. Patients with t(14;18) presented a lower mutation frequency than the rest of rearrangements, carrying mutations in BCL2 and HIST1H1E, and associated with good-prognosis markers such as IGHV-M.
Funding:PI15/01471; CIBERONC CB16/12/00233; FEHH-Janssen(MHS); JCyL(MQÁ)
Mateos:Janssen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Takeda: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Celgene: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; GSK: Consultancy, Membership on an entity's Board of Directors or advisory committees; Abbvie: Consultancy, Membership on an entity's Board of Directors or advisory committees; Amgen: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees; GSK: Consultancy, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal